Pathology: Part I (A walk around my brainstem)
How craniocervical instability and brainstem compression might have caused my ME symptoms
TL:DR? Here’s a brief summary: If you squish the brainstem from the front or the back, it could plausibly cause symptoms of dizziness, vertigo, sound sensitivity, GI dysfunction, immune dysfunction, POTS, sleep disturbance, facial numbness, chronic inflammation and a bunch of other symptoms. If you can relieve that pressure, it is plausible that it can help improve or resolve those symptoms.
In the last set of articles in my CCI + tethered cord series, “Onset,” I examined how a severe mold exposure along with a viral infection could have weakened the ligaments in my neck, causing craniocervical instability (CCI). I wrote about how a wide range of factors that weaken connective tissue might also contribute.
In this next set of articles, I explore how CCI and tethered cord syndrome, through their effects on the brain, brainstem and spinal cord, could theoretically cause a symptom complex similar, perhaps identical, to that described by myalgic encephalomyelitis (ME) diagnostic criteria. I’ll look at the anatomy of the brainstem, the pathophysiology of intracranial hypertension and spinal compression or strain, and the overlap — and differences — between CCI symptoms and our various definitions of ME. This first article focuses on the anatomy of the brainstem.
There are many symptoms people with ME experience as global, to the brain or to the body as a whole. These symptoms include post-exertional malaise, muscle weakness or fatigability, “brain fog,” and problems of blood flow. This article is not about those symptoms. Rather, it is about the many symptoms ME patients frequently experience that can be plausibly localized to specific areas of the brain, namely circuits in the brainstem and several of the cranial nerves that arise from or connect to it. Together, the brainstem and cranial nerves are responsible for the body’s basic sensory processing and autonomic functions, as well as motor control of the muscles of the throat, jaw, face, ears and eyes. To understand this anatomy is to understand how CCI could cause many of the symptoms of ME.
That the brainstem is involved in the pathophysiology of ME already has some evidence. Researchers have found evidence of brainstem hypoperfusion (low blood flow) and inflammation. (Two major studies currently underway, one by Mike VanElzakker at Harvard and another by Jarred Younger at the University of Alabama — Birmingham, should deepen our understanding.)
The pathology underlying this brainstem dysfunction is unknown, but it is possible that infection, toxic injury, inflammation, and structural abnormalities (skeletal, connective tissue, or vascular) could cause very similar symptoms, if they affected the same areas of the brain. My focus here will be on the possible effects of my structural diagnosis, CCI, on the function of my brainstem.
As none of the below symptoms are required for an ME diagnosis, it’s unknown how common they are among people with ME. However, many of them are included in the “stricter” diagnostic criteria, such as the Canadian Consensus Criteria and the International Consensus Criteria, as well as in the descriptions of ME outbreaks. Many of these symptoms also constitute cervicomedullary syndrome, a concept defined by a group of clinicians and researchers at the 2014 Chiari & Syringomyelia Foundation “Colloquium on Basilar Impression and Craniovertebral Instability,” among them surgeons who treat craniocervical junction abnormalities like Chiari or CCI.
The brainstem
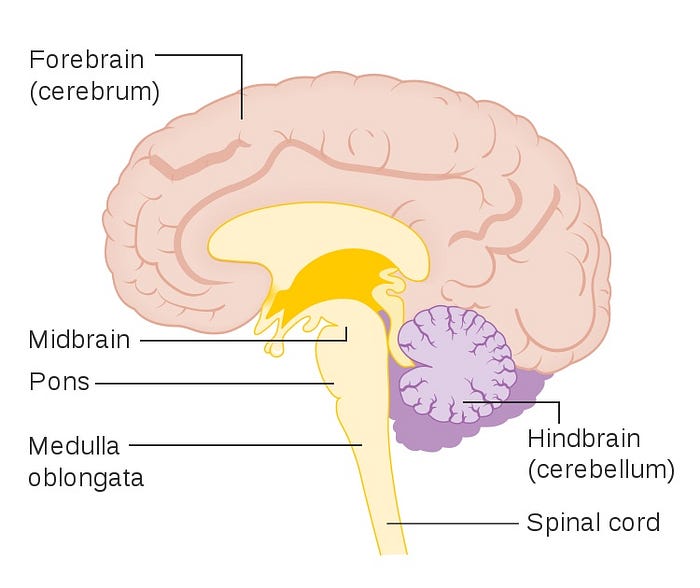
Unless you’re a doctor or a neuroscientist, this article is going to ask you to learn a lot of new terms. I encourage you to read this more than once, relate the terms to the diagrams, and look up things that you want to learn more about. Also think about how your specific pattern of symptoms might relate to the geography of your brain. Alright, here goes.
The brainstem is located at the bottom of the brain and is divided into three sections: the midbrain, pons and medulla oblongata. The medulla oblongata ends at the foramen magnum, the largest opening at the base of the skull, where it becomes the spinal cord. There is no real, gross anatomical distinction between the spinal cord and the brainstem: the two are continuous. In fact, as we think about how upper cervical spine problems could cause such profound brainstem dysfunction, it might be more helpful — and accurate — to think of the brainstem as the part of the spinal cord that is inside your skull rather than as a part of your brain.
The brainstem and spinal cord share fundamental structural and functional commonalities that have origins in embryonic development. Both have motor neurons in the front of the cord and sensory neurons in the back. Like the spinal cord, the brainstem has a number of nerves that branch off from it. These cranial nerves receive signals from other parts of the body and send “commands” back down those same nerves.
The twelve cranial nerves and their nuclei
There are twelve cranial nerves in total. Ten of them arise from the brain stem. The olfactory (I) and optic (II) nerves arise from the cerebrum and are responsible for our sense of smell and sight. The oculomotor (III) and trochlear (IV) nerves arise from the uppermost section of the brainstem, the midbrain. Together, they are responsible for most the eye’s motor movements. The trigeminal (V), abducens (VI), and facial (VII) nerves arise from the middle of the brainstem, the pons. The trigeminal is responsible for most of the face’s sensation and motor control of the jaw, while the facial nerve governs the muscles of facial expression. The facial nerve also plays a role in hearing as well as our sense of taste. The abducens controls the remaining eye movement, namely lateral motion of the eye. The vestibulocholear nerve (VIII) arises from the inner ear and connects to the pons. It has two branches, one responsible for our sense of balance and the other, hearing. Finally, the glossopharyngeal (IX), vagus (X), spinal accessory (XI) and hypoglossal (XII) nerves arise from the medulla oblongata. They are responsible for our sense of taste, gag reflex, tongue movements, swallowing and autonomic function, including heart rate, blood pressure, immune response and gastrointestinal motility, along with many other functions.

Most of these nerves have, in a sense, two copies: one carrying information from various sensory organs like the eyes and ears to the brainstem (afferent neurons), and one carrying information from the brainstem back to those organs (efferent neurons). The incoming information is processed and interpreted in the brainstem’s nuclei, areas of gray matter associated with one or more of these nerves. You can think of a nucleus as a sort of mini-processor. Information can then be sent back to the body in the form of the basic reflexes that govern functions like breathing or heart rate, and/or to other parts of the brain for higher-order processing or response. Nuclei related to motor processing tend to be located in the front of the brainstem (also called anterior or ventral), while areas related to sensory processing tend to be located at the back (posterior, dorsal).
Mapping brainstem & cranial nerve dysfunction
Here’s where things get interesting. I decided to try to map all of the symptoms I had prior to surgery to these cranial nerves and to the nuclei that interpret their information. Many of these symptoms correspond with either what is known about these regions’ functions or what happens when they are damaged in other conditions. For me, the “action” seems to be around cranial nerves VII to X and XII and/or their nuclei, which as you can see from the drawing below, are all anatomically quite proximate.

Geometry of brainstem compression
It can be difficult to distinguish between a symptom caused by a dysfunctional nerve (highlighted above and below in green) and a symptom caused by dysfunction of the nuclei that processes that nerve’s information (highlighted above and below in red). We know from the medical literature that either can cause almost identical symptoms. This may be why so many different upper cervical problems look alike.
For example, basilar invagination (which can occur with craniocervical instability) is a condition where the odontoid process, a bony protrusion of the front of the second vertebra (the axis), migrates upwards, narrowing the space the brainstem has to pass through the foramen magnum. It can also “kink” the front of the brainstem, causing ventral brainstem compression. In addition, a retroflexed odontoid might stretch some of the cranial nerves as they enter or exit the brainstem from the front. The transverse ligament is supposed to prevent this from happening but can become compromised in patients with connective tissue disorders. This phenomenon can be diagnosed via an MRI measurement called the clivo-axial angle. Its symptoms are very similar to that of Chiari malformation, where the descent of the tonsils of the cerebellum put pressure on the brainstem from the back. (Some very lucky people have both.)


Nearly all of the 63 ME patients who have been diagnosed with CCI in the last few months have an abnormal clivo-axial angle, a sign of possible ventral brainstem compression. I, however, did not have an abnormal clivo-axial angle. I did not have basilar invagination. I did not have a retroflexed odontoid. My symptoms did not get markedly worse with flexing or extending my head, as happens to many people who have retroflexed odontoids. This is unusual. (My symptoms did get severely worse when turned my head.)
I had cranial settling (vertical instability). Cranial settling would have the effect of modestly decreasing the space the brainstem and cerebellum have to share, conceivably resulting in dorsal brainstem compression by the cerebellum. Moreover, following my thyroid surgery, all of my symptoms — notably, my problems initiating respiration — could be triggered whenever I laid on the back of my head. For these reasons, I’m going to orient the exploration of my case around the nuclei located on the back (dorsal side) of the brain stem, from top to bottom.
How compression can cause brainstem or nerve dysfunction
This introduces one more important concept: a nerve or region of the brain does not need to have a lesion or any other visible damage in order to function improperly. Any form of physical stress to nervous tissue, whether compression, tension or sheer stress, can cause problems. This is because when a neuron is stretched or compressed, the shape of the membrane changes, disrupting homeostasis. This can have profound implications for cellular metabolism, electrolyte balance, and inflammation, as well as the neuron’s ability to conduct information via neurotransmitters and electrical impulses. The good news is that the effects of chronic physical stress can be reversible in many cases, if the cause can be identified and corrected.
It’s important to keep in mind that my diagnosis — craniocervical instability — is not the only way that the brainstem, cranial nerves and their functions can become compromised. As I have written above, any one symptom or even cluster of symptoms can have multiple causes. However, in my own case, the clustering of so many different symptoms in the same part of the brain, a diagnosis that explains how that part of the brain was compromised, and the complete resolution of all of my symptoms following surgery strongly point to brainstem dysfunction as the heart of my symptom complex.
How I think my brainstem was affected by CCI

Abducent nucleus (lateral eye movement)
The abducent nerve controls the movement of the lateral rectus muscle in humans, which is responsible for outward gaze. If damaged, it can cause double vision (diplopia) and gaze-induced horizontal nystagmus, a condition where the moves rapidly from side to side.
I do not recall ever having had double vision, but it can be a symptom of both Chiari Malformation and craniocervical instability (as well as many other things).
Internal genu of the facial nerve (facial expression and sound sensitivity)
The facial nerve controls the muscles of facial expression. It also innervates the stapedius, a 1mm long muscle in the middle ear. The stapedius dampens the movement of the stampedes bone, preventing excessive movement and thus modulating the amplitude of sound waves as they pass from the outside external environment to the inner ear. If the facial nerve is damaged or dysfunctional, it can cause Bell’s Palsy as well as hyperacusis (sound sensitivity), also sometimes a symptom of Bell’s Palsy.
Prior to surgery, I was almost constantly sensitive to sound, but especially during crashes. I would also occasionally have transient facial symptoms, such as numbness on the right side of my face. The right side of my mouth might be pulled downwards or snarled upwards for seconds to a few minutes. (Facial nerve damage usually occurs on one side of the face.)
Vestibular nuclei (spatial orientation and balance)
The vestibular nerve (a branch of the vestibulocochlear nerve) transmits information about balance from the inner ear, such as the position of our head relative to gravity. A collection of neurons in the back of the brainstem called the vestibular nuclei then transform this information into what we experience as our conscious sense of where our bodies are in space.
Through these nuclei’s connection to parts of the brainstem governing autonomic control, such as the dorsal/posterior vagus nerve nucleus and parts of the solitary tract, it also helps us to maintain stable blood pressure during movement, such as when you move from a seated to standing position. Through its connection to parts of the brainstem regulating eye movement, it also helps the eyes automatically make fine adjustments based on movement, so that you a) don’t get dizzy and b) have continuous and accurate binocular vision, even when in motion. Finally, it plays a role in spatial memory and spatial navigation.
Damage to the nerve can cause problems with dizziness, balance, vertigo, an inability to remain upright, and horizontal nystagmus — all symptoms associated with craniocervical junction abnormalities such as craniocervical instability or Chiari Malformation.
For me, this manifested initially as balance problems, which were worst at the beginning of my illness. However, the vestibular system has a remarkable ability to adapt, even when there is overt nerve damage. My balance problems eventually went away. What remained was intermittent dizziness, especially when moving from a seated to standing position, as well as the inability to orient myself while in motion. Prior to my fusion, going in reverse in the car, turning in circles in my wheelchair, or even scrolling too quickly through a page on my iPad, were all impossible. It could trigger symptoms ranging from motion sickness to full-on, sensory overload meltdown. I no longer have any problems with balance or motion.
Dorsal cochlear nucleus (complex auditory processing)
Along with the ventral (anterior) cochlear nucleus (the one closer to the front of the brainstem), the dorsal (posterior) cochlear nucleus interprets information transmitted from the inner ear by the cochlear branch of the vestibulocochlear nerve. However, rather than simply compiling and transferring the information, as the ventral cochlear nucleus does, the dorsal cochlear nucleus is thought to be responsible for more complex, second order auditory processing. This includes functions that are miraculous if you stop to think about them, such as our ability to place sound in a location in space as well as to improve the signal to noise ratio of auditory inputs, for example, isolating a voice from background sounds.
The latter was a large part of my sensory processing challenges. In addition to hyperacusis (sound sensitivity), I experienced a phenomenon where the voice of someone speaking 50 feet away sounded as loud as the person sitting next to me. It made it impossible to be in noisy, crowded places: the music blaring, the silverware clanking, the dozen or so simultaneous conversations, would all register at the same volume, as though coming from the same distance. Subjectively, I found this very confusing and it would also “crash” me.
Lastly, my tinnitus. It is not yet understood what causes tinnitus in patients with craniocervical junction problems, but there is some work suggesting that tinnitus might be a symptom of dorsal cochlear nucleus dysfunction, vestibular nucleus dysfunction, or both. My tinnitus along with all of my auditory processing problems disappeared immediately following my fusion surgery.
Solitary tract nucleus (interprets cardiovascular, respiratory and gastrointestinal signals)
The solitary tract nucleus, located in the medulla oblongata, is a sensory processing center for a wide range of taste and visceral signals from the facial, vagus and glossopharyngeal nerves. It also contains the dorsal respiratory group (DRG), a collection of neurons responsible for initiating breathing.
As the brain stem’s primary “relay station,” the signals received in the solitary tract nucleus are then integrated with other data and used to initiate reflexes that help regulate cardiovascular function, respiration, and gastrointestinal motility.
For example, the glossopharyngeal nerve connects to the carotid bodies, clusters of chemoreceptors in the carotid artery that measure the oxygen and carbon dioxide concentrations, pH and temperature of our blood. (Think: built-in oximeter, only much cooler!) It also connects to the carotid sinuses, a cluster of baroreceptors that measure our blood pressure. Any disruption to our body’s ability to accurately take or integrate these measurements could contribute to abnormal body temperature, heart rate or blood pressure. If these signals cannot be competently integrated with the vestibular nuclei, it might contribute to a worsening of symptoms with posture. If these signals cannot competently communicate with the DRG, it might mean that respiration would be initiated only after an abnormal rise in carbon dioxide (which is precisely what happened to me). The vagus nerve, meanwhile, transfers chemoreceptor and baroreceptor information from the aortic arch and from visceral receptors (e.g., stretch receptors) in the lungs, gastrointestinal system, and other organs, helping to regulate heart rate, peristalsis, normal gastrointestinal motility, and our sense of satiety.
The solitary tract nucleus also plays an important role in the immune system’s homeostasis. When it detects, via the vagus nerve, pro-inflammatory cytokines such as tumor necrosis factor-alpha or interleukin 1-beta, it triggers both glial cell activation within the central nervous system as well as the general innate immune response, sometimes called the sickness response. At the same time, via its connections to the hypothalamus, it plays a role in the release of corticosteroids, which have anti-inflammatory properties, from the adrenal glands (i.e., the HPA axis).
Dorsal motor nucleus of the vagus nerve (autonomic reflexes of heart, gastrointestinal tract and other organs)
If the solitary tract nucleus receives information from the arteries, heart, gastrointestinal tract and other organs via the vagus nerve, the dorsal motor nucleus of the vagus nerve (DMV) takes that information and transmits commands back down the vagus nerve. In other words, it tells those organs what to do in response. Through this processor, the vagus nerve influences everything from the secretion of stomach acid and movements of our GI tract, to the inhibition of tumor necrosis factors, pro-inflammatory cytokines released from the spleen, to the amount of insulin the pancreas secretes.
80% of the neurons in the DMV have projections into the stomach. Most of these neurons are cholinergic (that is, are neurons that primarily use the neurotransmitter acetylcholine). This may be why some patients report significant improvements in gastrointestinal function with Mestinon. Mestinon is an acetylcholinesterase inhibitor, which means it inhibits the enzyme that breaks down acetylcholine, thus raising acetylcholine levels. Increasing acetylcholine might, in essence, boost the signal of a dysfunctional DMV (or vagus nerve).
The DMV also influences contractability of the left ventricle of the heart. Abnormalities of left ventricle contractability/relaxation can contribute to preload failure. This may help explain why people with ME/CFS (or fibromyalgia or Ehlers-Danlos Syndrome) who have cardiac preload failure and exercise intolerance might also benefit from Mestinon.
In short, all of the autonomic symptoms that might plausibly result from dysfunction of the solitary tract nucleus and dorsal motor nucleus of the vagus nerve— postural orthostatic tachycardia, impaired GI motility, poor temperature regulation, and abnormal immune response— resolved with my craniocervical fusion. Mestinon normalized my gastrointestinal function and reduced my exercise intolerance, but since my fusion, I no longer need to take it. I no longer have POTS, my body temperature is always normal, and I never feel cold. My gut works like a dream, and since my surgery, I’ve had two colds, the first and only “normal” bouts of sickness in eight years.
Hypoglossal nucleus (tongue movements, swallowing)
Lastly, the hypoglossal nucleus is responsible for the movements of the tongue. Dysfunction to the hypoglossal nucleus or nerve might cause difficulty swallowing (dysphagia), a symptom of craniocervical junction abnormalities. I never noticed any difficulty swallowing, but sometimes, rarely and during specific episodes, I would stick out my tongue without any intention or control. I might also occasionally slur my speech.
I don’t have much to say about this particularly odd symptom other than now, if I ever stick out my tongue, it’s only because I mean to!
Wait, how did you figure all this out?
These ideas are not exactly novel. Many of the above symptoms are symptoms of the proposed entity, “Cervical medullary syndrome,” a form of brainstem dysfunction caused by abnormalities in the surrounding skeletal structures. These abnormalities are thought to exert pathological physical stress on the brainstem and include Chiari Malformation, craniocervical instability, and atlantoaxial instability.
Moreover, Mike VanElzakker has long emphasized the role of the vagus nerve and brainstem in ME. What I have not seen before is an attempt to map specific symptoms to the microanatomy of the brainstem. I personally found it a helpful exercise for more deeply understanding how the brainstem works. Even assuming that my hypothesis about my case is generally correct, I am hardly an expert, and there are more than a few things I have probably gotten wrong in the details (or that perhaps, are not even yet known). Here are some of the in-the-weeds questions I am still trying to answer:
- Are there any circuits in the brainstem that play a role in regulating *cerebral* blood flow? I am primarily trying to understand why I woke up after surgery with rosy cheeks and subjectively normal blood flow following years of looking sickly and pale. Brain hypoperfusion is thought to play a role in ME but may not be directly related to POTS or orthostatic hypotension. After all, even with significant swings in peripheral blood pressure, the body is thought to have many redundant mechanisms for maintaining cerebral blood flow within fairly narrow parameters. However, the contribution of neurogenic mechanisms (in other words, of the brain’s overt control of cerebral blood flow) is thought to be minor. (I believe there are several possible indirect mechanisms that might explain restoration of blood flow post-surgery, which I’ll explore in my next Medium piece.)
- Nucleus of the solitary tract v. dorsal motor nucleus of the vagus nerve: What is the difference between symptoms of nucleus of the solitary tract damage/dysfunction v. dorsal motor of the vagus nerve damage/dysfunction? (They are located right next to each other, and using the literature to clearly distinguish between problems caused by signals coming into the brainstem via the vagus nerve versus signals going out isn’t always easy.)
- Ventral v. dorsal compression: Can compression of the brainstem from the back (e.g., caused by Chiari malformation) v. deformation of the cranial nerves and ventral brainstem compression (e.g., caused by basilar invagination) result in very similar yet distinct symptom presentations?
What about intracranial hypertension?
There is some evidence that at least a subset of people with ME/CFS diagnoses have idiopathic intracranial hypertension (IIH). Like CCI, it has been associated with Ehlers-Danlos Syndrome, can have structural, infectious, and other causes, can co-occur with CCJ abnormalities that obstruct spinal fluid or blood flow, and can cause many of the same cranial nerve compressions, and thus symptoms, described above.
Prior to my fusion surgery, I had intracranial hypertension (as diagnosed via MRI signs and an intracranial pressure bolt). It was caused by cranial settling, a feature of some kinds if craniocervical instability. As such, while there are some symptoms I can confidently ascribe to IIH, such as pressure in my head and behind my eyes, there are many symptoms that could plausibly have been caused by either some specific, focal compression of my brainstem due to instability, or by the global effects of elevated cranial pressure. Moreover, given that cranial settling caused the pressure, it’s difficult to say where the two mechanisms are even substantively different in my case. I do think IIH is an incredibly important topic in its own right, one I will dive into a bit more in a future article.
What about postural orthostatic tachycardia (POTS)?
I mention POTS in more than one section above. I cannot pretend to know what causes POTS, which likely has many possible causes. I only know that mine completely resolved following my craniocervical fusion surgery. It is quite possible that in my case, several different parts of the brainstem were involved: the vestibular nucleus, which interprets information about posture, the solitary tract nucleus, which receives signals about blood pressure, and the dorsal motor nucleus of the vagus nerve, which helps regulate heart rate. (These possible connections are discussed, for example, in this experiment.)
What about sleep-wake cycle dysfunction?
A substantial proportion of ME patients have “unrefreshing sleep” due to disturbances in their sleep architecture. Some may have such significant circadian rhythm drifts that no matter what they do, they cannot wake up before two o’clock in the afternoon or go to bed before the sun rises.
Sleep is one thing I never had a problem with and I may have an explanation for this. As I wrote above, most of the 63 ME/CFS patients who have been diagnosed with craniocervical instability since Jeff Wood and I came out about our diagnoses have abnormal clivo-axial angles (< 135 degrees). This means that their brainstems may be compressed or deformed from the front. I suspect my brainstem compression was from the back.
Our circadian rhythms as well as the initiation, pattern, and resolution of sleep involve many different parts of the brain but the brainstem plays an important role. In particular, an area in the front of the brainstem called the ventral tegmental area (VTA).
Could ventral (front) brainstem compression, then, cause sleep-wake cycle disturbances while dorsal (back) brainstem compression might not?
What about post-exertional malaise and brain fog?
The above regions of the brainstem and associated symptoms encapsulate nearly all of the symptoms I had for eight long years, save: muscle fatigability, post-exertional malaise and “brain fog.” These were also very likely caused in my case by craniocervical instability, but I suspect through more indirect mechanisms. I’ll explain exactly how this might have worked in the next few Medium pieces.
What does this have to do with crashing?
One of the weirder dynamics of this disease is how, particularly if we are severely affected or in a fragile state, an event that triggers one symptom can make all symptoms worse. A pile of dishes can come crashing off the kitchen counter, and suddenly our body temperature will go haywire and we’ll have diarrhea. A bad jolt in a car and we’ll get extremely sound sensitive and feel as though we have a fever.
When we consider how and, crucially, where all of this information is processed, I believe the relationship between these “strange” symptoms starts to become easier to understand.
I also believe involvement of the brainstem, whether because of craniocervical instability or some other cause, might also explain why our symptom presentations can be so varied and seemingly complex, even if the underlying mechanism(s) are sometimes surprisingly straightforward.
What about my symptom X?
If you have a symptom that is not included among the symptoms above, why not do some research and see if that symptom relates to a known function or dysfunction of the brainstem? If it does, it may be a clue. And if it doesn’t, that might be a clue, too! Either way, your experience can help inform where this model might be strong or weak, where it might be useful or where it might be incomplete, and what it might fail to explain entirely.
Thank you to all the PwME on Facebook who contributed to and helped improve the clarity of this article. This is a monster article with a lot of factual detail. Consider it a 1.0 version. If you see any important errors or omissions, please drop me a line!
To be continued in Pathology: Part II (PEM and muscle fatigability)
Read all the posts in my CCI + tethered cord series
Read this disclaimer. Crucially, surgery carries risks and it’s important to remember that in medicine, the same exact symptoms can have multiple, different causes. We have no idea how prevalent CCI is in our community and there’s been no research into its relationship with ME. We do know that it is more common among patients with EDS.
